Endometriosis is a condition where tissue similar to the inner lining of the womb (endometrium) is found elsewhere, usually in the pelvis around the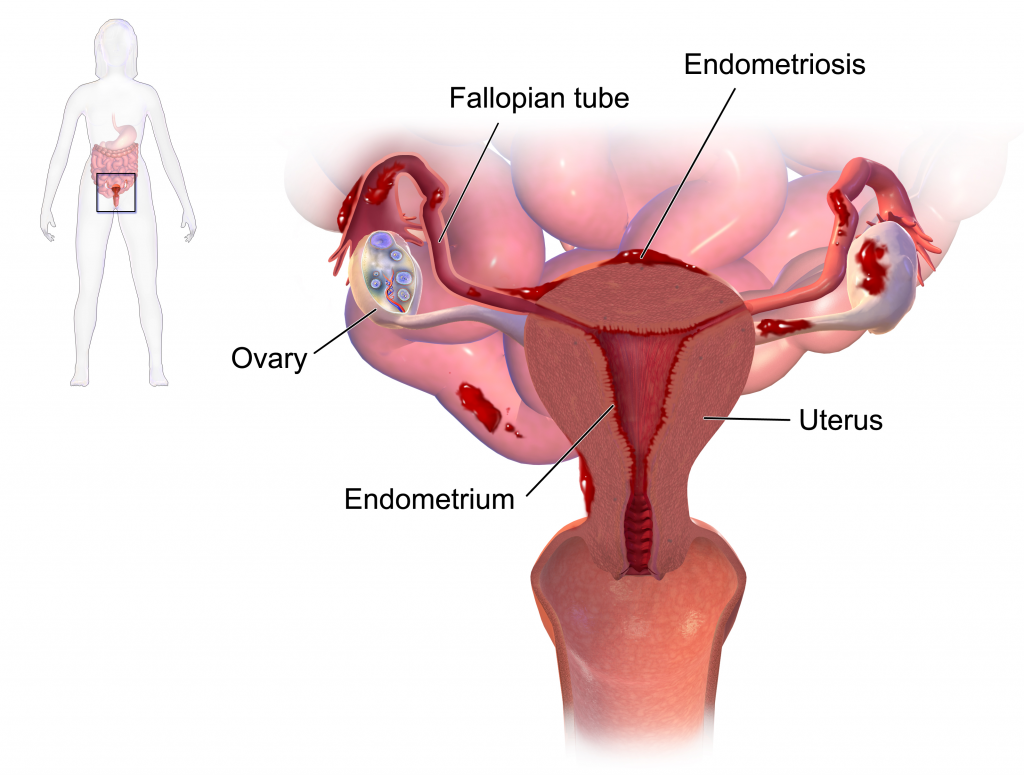 womb, ovaries and fallopian tubes. It is a very common condition, affecting around 1 in 10 women, approximately 176 million women worldwide. You are more likely to develop endometriosis if your mother or sister has had it. Endometriosis affects women during their reproductive years. It can be a long-term condition, that can have a significant impact on your general physical health, emotional wellbeing and daily routine.
womb, ovaries and fallopian tubes. It is a very common condition, affecting around 1 in 10 women, approximately 176 million women worldwide. You are more likely to develop endometriosis if your mother or sister has had it. Endometriosis affects women during their reproductive years. It can be a long-term condition, that can have a significant impact on your general physical health, emotional wellbeing and daily routine.
During normal monthly menstruation, the lining of the womb is shed via the vagina. With endometriosis the deposits of tissue outside the womb also bleed but this blood is trapped around the pelvic organs or under the surface of the tissues. This results in inflammation, pain and loss of tissue architecture due to scarring.
Symptoms may vary from person to person but may include the following:
- Painful periods
- Heavy, irregular periods
- Pelvic pain not related to the periods
- Pain during or after sexual intercourse
- Lower back pain
- Abdominal pain
- Pain when passing urine
- Pain when passing stool
- Bleeding from the bowel or the bladder during menstruation
- Fertility problems
- Long-term fatigue
- Constipation, diarrhoea, bloating around the time of menses
- Migraines
- Difficulty breathing – a very rare complication
Endometriosis can cause pain that occurs in a regular pattern, becoming worse before and during your period. Some women experience pain all the time but for others it may come and go. The pain may improve during pregnancy and sometimes it may disappear without any treatment. Treatment may relieve the symptoms but relapses may still occur.
Endometriosis is a difficult condition to diagnose for a variety of reasons. The symptoms of the condition are wide, varied and differ from woman to woman. Symptoms of endometriosis share characteristics with other conditions, such as irritable bowel syndrome (IBS) and pelvic inflammatory disease (PID). Thus, at your consultation you may be asked about the characteristics of the pain in relation to your menses and sexual activity, bowel or bladder symptoms and previous sexually transmitted diseases.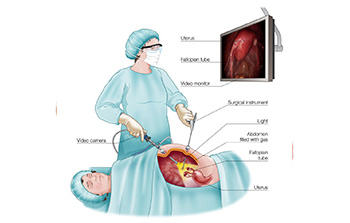
Ultrasound Scan An ultrasound is usually the first imaging test requested, this may show endometrial cysts in the ovaries(endometriomas) or significant deposits in the deep pelvis. Additionally, other conditions like uterine fibroids might also be detected.
Laparoscopy Definitive diagnosis of endometriosis is done surgically via laparoscopy (keyhole surgery). A small telescope is used to visualise the female reproductive organs to determine if any endometriotic deposits are present. A biopsy may be taken to confirm the diagnosis but, in most cases, a see and treat approach is adopted. This involves removing endometriomas, deposits and separating adhesions during the initial surgery. Additional procedures such as the dye test may be performed at this time if there is a history of infertility.
Analgesics (pain medication) – Drugs such as Panadol or Motrin may be used to simply relieve the pain of endometriosis but don’t cause any disease regression.
Hormonal Therapies- These treatments reduce or stop ovulation (the release of an egg from the ovary) and therefore allow the endometriosis to shrink by decreasing estrogen stimulation. Some hormone treatments that may be offered are listed below.
The combined oral contraceptive (COC) pill, given continuously for three months, without the normal pill free break. This stops ovulation and lightens or abolishes menses, leading to less painful periods.
Progestogens in the form of pills, long acting injection or implants are all used to stop ovulation, reduce estrogen production and treat endometriosis.
GnRh agonist work at the level of the brain to stop estrogen production and effectively stop the progression of endometriosis, however it’s side effect profile limits treatment to 6 months.
